Types Of MS
The course of MS is unpredictable.
Some people are minimally affected by the disease while others have rapid progression to total disability, with most people fitting between these two extremes.
Although every individual will experience a different combination of MS symptoms, there are a number of characteristic patterns relating to the course of the disease.
The term “Clinically Isolated Syndrome” is often used when a person has had only a single clinical attack without other evidence to establish a diagnosis of MS.

In general, the four typical patterns of MS are:
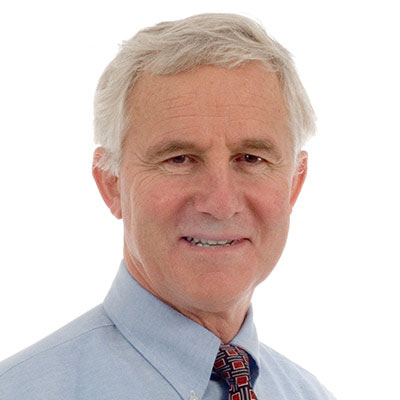
RRMS is the most common form of the disease. It is characterised by clearly defined acute attacks with full recovery (1a) or with residual deficit upon recovery (1b).
Periods between disease relapses are characterised by a lack of disease progression. Approximately 85% of people with MS begin with a relapsing-remitting course.
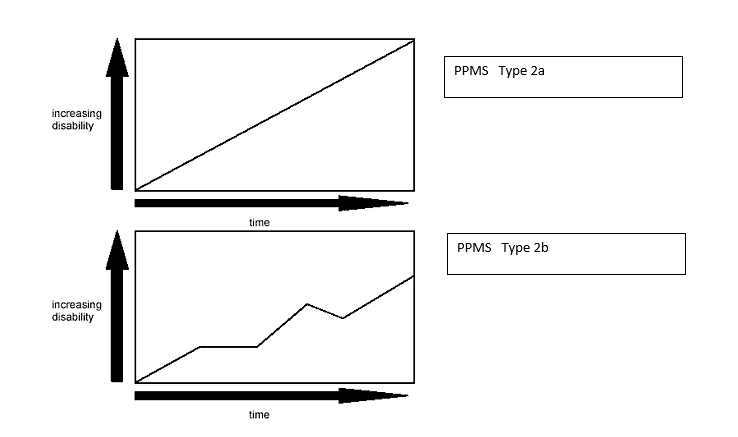
PPMS is characterised by gradual progression of disability from onset, without plateaus or remissions (2a) or with occasional plateaus and temporary minor improvements (2b).
A person with PPMS, by definition, does not experience acute attacks, before gradually worsening. Of people diagnosed with MS, only about 10% have PPMS.
In addition, PPMS may be difficult to distinguish from other degenerative CNS diseases so that often the diagnosis may be delayed for some time after the onset of neurological symptoms, and at a time when the person is already living with significant disability.
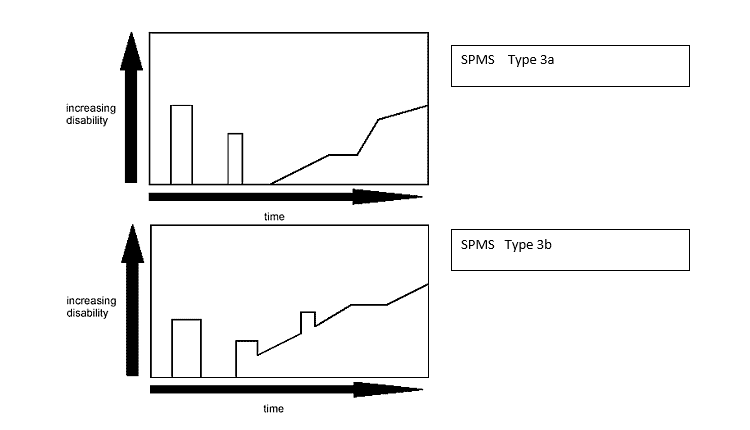
SPMS begins with an initial relapsing-remitting disease course, followed by gradual progression of disability (3a) that may include occasional relapses and minor remissions and plateaus (3b).
Secondary progressive disease tends to develop earlier in those who have less recovery following attacks. Once SPMS is established, relapses are less likely to occur, although there may be fluctuation in symptoms, not clearly related to new inflammation.
According to some natural history studies, of the 85% who start with relapsing-remitting disease, more than 50% will develop SPMS within 10 years and 90% within 25 years.
More recent natural history studies (perhaps because of the use of MRI to assist in the diagnosis) suggest a more benign outlook than these numbers suggest.
There is also increasing evidence that early treatment of RRMS with disease modifying therapy may reduce the development of SPMS. Nevertheless, many patients with RRMS ultimately develop SPMS.
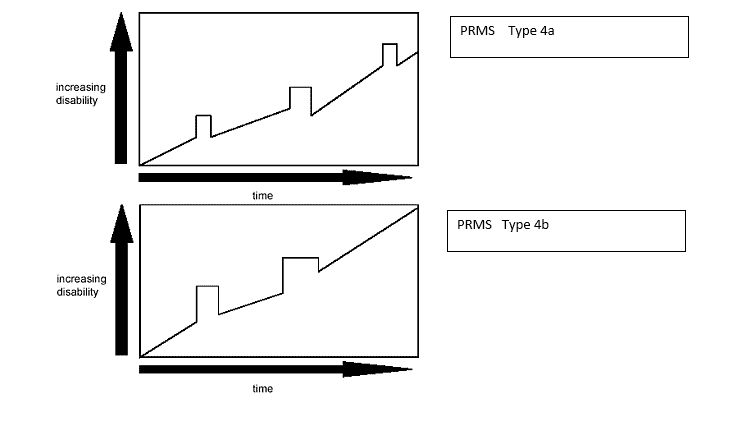
PRMS, which is the least common disease course, shows progression of disability from onset but with later acute relapses, with (4a) or without (4b) full recovery to the pre-relapse state.
Approximately 5% of people with MS appear to have PRMS at diagnosis. Not infrequently a patient may be initially diagnosed as having PPMS and then will experience an acute attack, thereby establishing the diagnosis of PRMS.